List of recent progress in bioengineering research
- Categories:Industry news
- Author:
- Origin:
- Time of issue:2018-09-28
- Views:37
(Summary description)1. Nat Commun: Bioengineering miniature silkworm cocoons to protect drug molecules has miraculous effects!
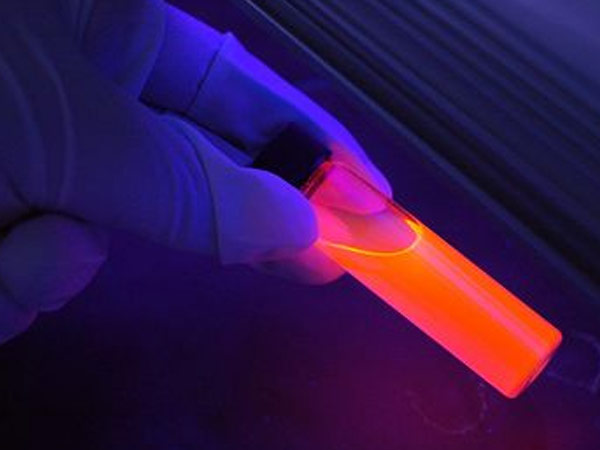
Scientists have created a tiny silkworm cocoon that protects sensitive drug molecules from degradation during storage and release. They hope the technology will extend the shelf life of drugs and help treat cancer, neurodegenerative diseases and more.
For scientists, finding inspiration from nature to facilitate human life is a common method. In the past, scientists have been inspired by enzymatic reactions in nature to produce energy and by cacti to store water. Today, we use the natural properties of silkworm pupae to create carriers suitable for small molecules. "Many drugs have excellent therapeutic effects, but have low stability and are difficult to store. This is a common problem in medical practice," said the study's lead author, Tuomas Knowles from the University of Cambridge. Therefore, they hoped that the cocoons could help prolong the lifespan of the drug molecules. Because silk is a biodegradable remnant and is inexpensive to produce, it has been used to make other surgical supplies, including brain implants, optical devices, Xibao Home, and sticky glue, to name a few. The safety of the modified material has been proven.
In order to transform silkworm cocoons for human use, the researchers used a unique micro-engineering technology to produce a miniature simulated silkworm cocoon, which is one-thousandth the volume of a natural silkworm cocoon. Afterwards, the researchers tested the protective effect of the miniature silkworm cocoons on antibodies. Antibodies are known to be the most difficult type of drug to preserve. At higher concentrations, antibodies tend to aggregate and it is difficult to maintain the original stability. "By wrapping the antibody inside a tiny silkworm cocoon, we were able to significantly enhance its lifespan and also expand the range of uses for antibody drugs," says Knowles. "We are very pleased that the engineered micromaterials have new uses."
The results were published in the journal Nature Communications.
2. Sci Trans Med: Successful expansion of engineered liver tissue after transplantation
Many diseases, including cirrhosis and hepatitis, can lead to liver failure. There are currently more than 17,000 patients in the United States suffering from liver failure and anxiously awaiting liver transplants. However, available liver donors are in short supply.
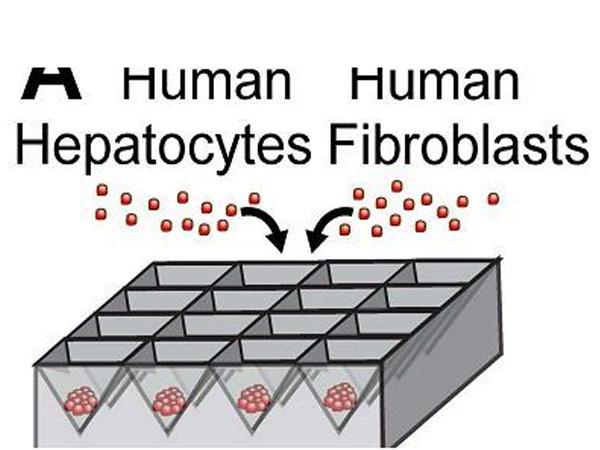
To address the shortage of donors, the researchers successfully developed engineered liver tissue. That is, by encapsulating three different types of cells in a biodegradable tissue framework. In a mouse model of liver injury disease, the researchers found that the engineered liver expanded about 50-fold after being transplanted into the mouse abdominal cavity, and was eventually able to perform full liver function.
This engineered liver could help millions of patients suffering from chronic liver disease who do not have a suitable donor. The results were published in the latest issue of the journal Science Translational Medicine.
"These patients do not need a donor transplant urgently, but they do have liver disease, and if the engineered liver can end up in the clinic, it will help these patients at the same time," said Dr. Kelly Stevens, an author on the paper.
In 2011, Bhatia et al. developed an engineered tissue framework that can be transplanted into the abdominal cavity of mice. After that, the liver cells in the frame can integrate with the original circulatory system of the mouse, so as to obtain blood supply and realize the function of the liver. However, this structure can contain fewer than 1 million liver cells, whereas a healthy human liver has at least 100 billion cells. Bhatia believes that to help liver patients, at least 10% to 30% of the liver cells need to be transplanted.
To increase the number of liver cells, the researchers hoped that the initially transplanted liver cells would replicate themselves. "The liver is the only mature organ in our body that can proliferate," Bhatia said.
In collaboration with other researchers, Bhatia et al. placed hepatocytes, fibroblasts, and endothelial cells into miniature liver structures, and eventually allowed them to proliferate and differentiate in vivo to form a replacement liver.
When the engineered liver was transplanted into mice, it was able to be influenced by signals from the peripheral environment. These signals, including growth factors, enzymes, and other molecules, are naturally produced when the liver is damaged, and can activate endothelial cells to form blood vessels and activate liver cells to proliferate to a nearly 50-fold expansion into normal liver tissue.
The researchers believe that if the technology can enter clinical practice, it will offer new hope for the majority of liver patients waiting for transplants.
3. Nature: Heavy! Bioengineered human liver tissue developed to mimic natural development
I
List of recent progress in bioengineering research
(Summary description)1. Nat Commun: Bioengineering miniature silkworm cocoons to protect drug molecules has miraculous effects!
Scientists have created a tiny silkworm cocoon that protects sensitive drug molecules from degradation during storage and release. They hope the technology will extend the shelf life of drugs and help treat cancer, neurodegenerative diseases and more.
For scientists, finding inspiration from nature to facilitate human life is a common method. In the past, scientists have been inspired by enzymatic reactions in nature to produce energy and by cacti to store water. Today, we use the natural properties of silkworm pupae to create carriers suitable for small molecules. "Many drugs have excellent therapeutic effects, but have low stability and are difficult to store. This is a common problem in medical practice," said the study's lead author, Tuomas Knowles from the University of Cambridge. Therefore, they hoped that the cocoons could help prolong the lifespan of the drug molecules. Because silk is a biodegradable remnant and is inexpensive to produce, it has been used to make other surgical supplies, including brain implants, optical devices, Xibao Home, and sticky glue, to name a few. The safety of the modified material has been proven.
In order to transform silkworm cocoons for human use, the researchers used a unique micro-engineering technology to produce a miniature simulated silkworm cocoon, which is one-thousandth the volume of a natural silkworm cocoon. Afterwards, the researchers tested the protective effect of the miniature silkworm cocoons on antibodies. Antibodies are known to be the most difficult type of drug to preserve. At higher concentrations, antibodies tend to aggregate and it is difficult to maintain the original stability. "By wrapping the antibody inside a tiny silkworm cocoon, we were able to significantly enhance its lifespan and also expand the range of uses for antibody drugs," says Knowles. "We are very pleased that the engineered micromaterials have new uses."
The results were published in the journal Nature Communications.
2. Sci Trans Med: Successful expansion of engineered liver tissue after transplantation
Many diseases, including cirrhosis and hepatitis, can lead to liver failure. There are currently more than 17,000 patients in the United States suffering from liver failure and anxiously awaiting liver transplants. However, available liver donors are in short supply.
To address the shortage of donors, the researchers successfully developed engineered liver tissue. That is, by encapsulating three different types of cells in a biodegradable tissue framework. In a mouse model of liver injury disease, the researchers found that the engineered liver expanded about 50-fold after being transplanted into the mouse abdominal cavity, and was eventually able to perform full liver function.
This engineered liver could help millions of patients suffering from chronic liver disease who do not have a suitable donor. The results were published in the latest issue of the journal Science Translational Medicine.
"These patients do not need a donor transplant urgently, but they do have liver disease, and if the engineered liver can end up in the clinic, it will help these patients at the same time," said Dr. Kelly Stevens, an author on the paper.
In 2011, Bhatia et al. developed an engineered tissue framework that can be transplanted into the abdominal cavity of mice. After that, the liver cells in the frame can integrate with the original circulatory system of the mouse, so as to obtain blood supply and realize the function of the liver. However, this structure can contain fewer than 1 million liver cells, whereas a healthy human liver has at least 100 billion cells. Bhatia believes that to help liver patients, at least 10% to 30% of the liver cells need to be transplanted.
To increase the number of liver cells, the researchers hoped that the initially transplanted liver cells would replicate themselves. "The liver is the only mature organ in our body that can proliferate," Bhatia said.
In collaboration with other researchers, Bhatia et al. placed hepatocytes, fibroblasts, and endothelial cells into miniature liver structures, and eventually allowed them to proliferate and differentiate in vivo to form a replacement liver.
When the engineered liver was transplanted into mice, it was able to be influenced by signals from the peripheral environment. These signals, including growth factors, enzymes, and other molecules, are naturally produced when the liver is damaged, and can activate endothelial cells to form blood vessels and activate liver cells to proliferate to a nearly 50-fold expansion into normal liver tissue.
The researchers believe that if the technology can enter clinical practice, it will offer new hope for the majority of liver patients waiting for transplants.
3. Nature: Heavy! Bioengineered human liver tissue developed to mimic natural development
I
- Categories:Industry news
- Author:
- Origin:
- Time of issue:2018-09-28
- Views:37

Scientists have created a tiny silkworm cocoon that protects sensitive drug molecules from degradation during storage and release. They hope the technology will extend the shelf life of drugs and help treat cancer, neurodegenerative diseases and more.
For scientists, finding inspiration from nature to facilitate human life is a common method. In the past, scientists have been inspired by enzymatic reactions in nature to produce energy and by cacti to store water. Today, we use the natural properties of silkworm pupae to create carriers suitable for small molecules. "Many drugs have excellent therapeutic effects, but have low stability and are difficult to store. This is a common problem in medical practice," said the study's lead author, Tuomas Knowles from the University of Cambridge. Therefore, they hoped that the cocoons could help prolong the lifespan of the drug molecules. Because silk is a biodegradable remnant and is inexpensive to produce, it has been used to make other surgical supplies, including brain implants, optical devices, Xibao Home, and sticky glue, to name a few. The safety of the modified material has been proven.
In order to transform silkworm cocoons for human use, the researchers used a unique micro-engineering technology to produce a miniature simulated silkworm cocoon, which is one-thousandth the volume of a natural silkworm cocoon. Afterwards, the researchers tested the protective effect of the miniature silkworm cocoons on antibodies. Antibodies are known to be the most difficult type of drug to preserve. At higher concentrations, antibodies tend to aggregate and it is difficult to maintain the original stability. "By wrapping the antibody inside a tiny silkworm cocoon, we were able to significantly enhance its lifespan and also expand the range of uses for antibody drugs," says Knowles. "We are very pleased that the engineered micromaterials have new uses."
The results were published in the journal Nature Communications.
2. Sci Trans Med: Successful expansion of engineered liver tissue after transplantation
Many diseases, including cirrhosis and hepatitis, can lead to liver failure. There are currently more than 17,000 patients in the United States suffering from liver failure and anxiously awaiting liver transplants. However, available liver donors are in short supply.
To address the shortage of donors, the researchers successfully developed engineered liver tissue. That is, by encapsulating three different types of cells in a biodegradable tissue framework. In a mouse model of liver injury disease, the researchers found that the engineered liver expanded about 50-fold after being transplanted into the mouse abdominal cavity, and was eventually able to perform full liver function.
This engineered liver could help millions of patients suffering from chronic liver disease who do not have a suitable donor. The results were published in the latest issue of the journal Science Translational Medicine.
"These patients do not need a donor transplant urgently, but they do have liver disease, and if the engineered liver can end up in the clinic, it will help these patients at the same time," said Dr. Kelly Stevens, an author on the paper.
In 2011, Bhatia et al. developed an engineered tissue framework that can be transplanted into the abdominal cavity of mice. After that, the liver cells in the frame can integrate with the original circulatory system of the mouse, so as to obtain blood supply and realize the function of the liver. However, this structure can contain fewer than 1 million liver cells, whereas a healthy human liver has at least 100 billion cells. Bhatia believes that to help liver patients, at least 10% to 30% of the liver cells need to be transplanted.
To increase the number of liver cells, the researchers hoped that the initially transplanted liver cells would replicate themselves. "The liver is the only mature organ in our body that can proliferate," Bhatia said.
In collaboration with other researchers, Bhatia et al. placed hepatocytes, fibroblasts, and endothelial cells into miniature liver structures, and eventually allowed them to proliferate and differentiate in vivo to form a replacement liver.
When the engineered liver was transplanted into mice, it was able to be influenced by signals from the peripheral environment. These signals, including growth factors, enzymes, and other molecules, are naturally produced when the liver is damaged, and can activate endothelial cells to form blood vessels and activate liver cells to proliferate to a nearly 50-fold expansion into normal liver tissue.
The researchers believe that if the technology can enter clinical practice, it will offer new hope for the majority of liver patients waiting for transplants.
3. Nature: Heavy! Bioengineered human liver tissue developed to mimic natural development
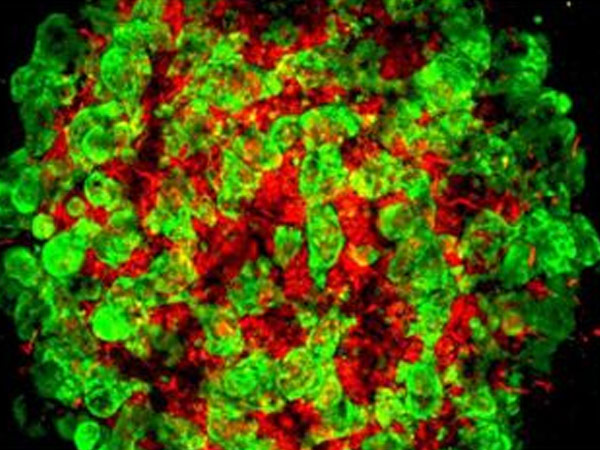
In a new study, researchers from Germany, the United States and Japan used bioengineered human liver tissue they developed to discover a previously unknown network of molecule-cell conversations that control the development of the liver organ, which greatly facilitates the use of human The effort of pluripotent stem cells to generate healthy, workable human liver tissue. They report that further molecular fine-tuning of their bioengineered human liver tissue is still required before they can be tested in clinical trials. The related research results were published online in the journal Nature on June 14, 2017, with the title of "Multilineage communication regulates human liver bud development from pluripotency". The corresponding authors of the paper are Dr. Takanori Takebe, researcher in the Division of Gastroenterology, Liver and Nutrition at Cincinnati Children's Medical Center, Dr. Barbara Treutlein, researcher at the Max Planck Institute for Evolutionary Anthropology, Germany, and Keisuke Sekine, researcher at the Department of Regenerative Medicine, Graduate School of Medicine, Yokohama City University, Japan. PhD.
The only current treatment for advanced liver disease is liver transplantation, however the number of livers obtained from deceased donors is limited. Based on this, a major goal of regenerative medicine is to obtain self-assembled human tissues, in which cells undergo a coordinated series of molecular events in precise time and space to form functional three-dimensional liver buds.
Elucidating the detailed details and context of molecular-cell cross-talk in embryonic endoderm development is critical to the therapeutic potential of this technique. The liver is formed in the embryonic endoderm.
"The ability to bioengineer transplantable livers and liver tissue could be of great benefit to patients with liver disease who need new and innovative treatments to save lives," Takebe said. "Our data allow us to understand the developing A new detailed understanding of the intercellular communication between hepatocytes has been obtained, and we have demonstrated that we are able to generate liver buds that are remarkably close to replicating that produced by human naturally developing fetal cells."
genetic blueprint
In the current study, the researchers used single-cell RNA sequencing (RNA-Seq) to monitor how individual cells changed when they were brought together in a three-dimensional environment. In this three-dimensional environment, vascular cells, connective tissue cells and liver cells undergo complex communication.
The main advantage of single-cell RNA-Seq technology is that it provides a blueprint of gene activity in each cell type. The researchers focused on drawing a complete picture of the active transcription factors, signaling molecules and receptors in each different cell before and after the cells were put together to form liver tissue.
The researchers report that they observed dramatic changes in molecular-cell communication and how the cells behave when grown together in a three-dimensional environment.
Single-cell RNA-Seq analysis also helped to compare 3D-engineered liver tissue generated from stem cells with naturally occurring human fetal and adult hepatocytes. The researchers observed that laboratory-grown liver buds had molecular and genetic profiles very similar to those found in naturally developing human hepatocytes.
In particular, they focused on revealing that cells produce a signaling protein that promotes blood vessel formation (ie, vascular endothelial growth factor, or VEGF) and a protein receptor that communicates with VEGF to help promote blood supply to the developing liver ( Molecular conversation between KDR receptors. The current study confirms that communication between VEGF and KDR plays a crucial role in directing liver tissue development and maturation.
The researchers noted that they observed this conversation during the development of mouse liver cells, natural human liver cells, and their bioengineered livers.
"Our data reveal very clearly that this conversation between different types of cells changes these cells in a way that might mimic what happens during human development," Trentlein said. There is still a lot to learn about how best to generate functional human liver tissue, but this study is a major advance in that direction."
Natural Tissue vs Bioengineered Tissue
The researchers noticed that the gene expression profiles in these produced liver buds, such as where and when genes were expressed, did not exactly match natural human hepatocytes. The remaining differences between natural and bioengineered tissues may arise from different developmental cues resulting from the unique microenvironment of cells in a dish and those in humans or animals.
The new cellular and molecular data found in the current issue will "be used in the future to further improve liver bud organoid formation" and "accurately reproduce all cell types in human fetal development," the researchers wrote. differentiation".
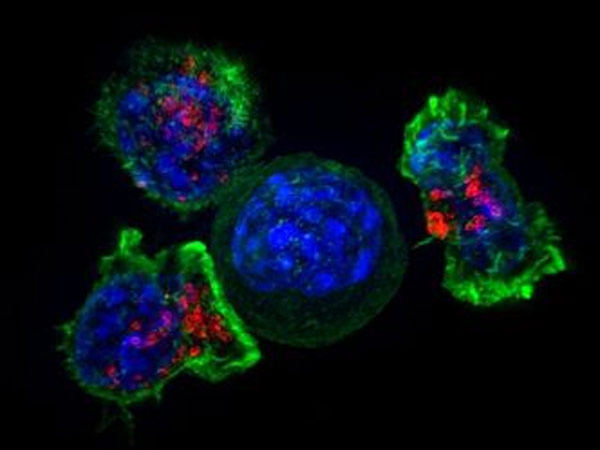
Studying E. coli may help scientists develop new tools to better detect cancer. A team of scientists from Griffith University's Glycomics Institute, the University of Adelaide and the University of Queensland explain their new findings in detail in a new study published today in Scientific Reports.
Professor Michael Jennings, from the Institute of Glycoomics, explained that E. coli can produce a toxin that binds to an unusual sugar on the cell surface, which is part of the cell surface carbohydrate (Neu5Gc), which is not found on normal cells. this sugar.
"The structure recognized by the toxin is a tumor antigen, a recognizable marker produced by tumor cells that can be used to detect and diagnose cancer."
The team then took the naturally occurring toxin and engineered it to change its composition so that it only specifically recognizes the sugar structure on the surface of tumor cells.
"The real innovation is that we've translated what we've discovered in the food poisoning infectious disease research project to be able to detect tumor antigens," Professor Jennings said.
And this tumor antigen can be produced by a series of tumors, such as breast and ovarian cancer.
"There's a saying in the scientific community that chance favors the brainy, and it's because we work with infectious disease and cancer researchers in the Institute that we have the chance to breed such opportunities and outcomes. When we discover this engineering We were all surprised when the toxin worked so well, we removed the useless binding domain and made it completely specific for this tumor antigen," he explained.
The level of Neu5Gc on the surface of tumor cells is very high, but normal cells hardly express the substance, so the detection of Neu5Gc means that the patient may have cancer.
The human body does not synthesize Neu5Gc itself, but we are able to absorb it through our daily diet such as red meat.
Professor Jennings explained that although more research is needed, it is important that this new tool can detect a range of cancers more sensitively.
5. Sci Adv: Bioengineering & Transplant Therapy Can Cure Type 1 Diabetes

Recently, researchers have been able to improve the success rate of suppressing islet cells in the treatment of type 1 diabetes by combining a novel hydrosol material with a protein that promotes blood vessel growth. In animal models, the technology was able to enhance the success of transplantation of insulin-secreting cells, restore insulin production in response to blood sugar levels, and treat diabetic symptoms in animals.
The technology could also aid in the treatment of patients who have had to have their pancreas removed due to pancreatitis or other inflammatory conditions. By combining the protein with the new material, the researchers compared the effect of inhibiting islet cells at different sites, the first systematic comparison of the effects of transplantation at different sites.
The results were published in the journal Science Advances.
Type 1 diabetes affects 1.25 million people in the United States, which is caused by the body's inability to produce insulin. To control the disease, patients must regularly check blood sugar levels and inject insulin to maintain blood sugar balance. But some patients also experience hypoglycemia, which can lead to serious health problems.
Previously, researchers used cells isolated from dead bodies for islet transplantation, but many of the transplanted islets rapidly died due to immune rejection. Despite decades of trials, the problem of immune rejection has not been resolved.
Garca et al. developed a class of degradable polymer hydrosols to transplant islet cells into diseased animals, and used this hydrosol to re-introduce VEGF factors into the body to promote the proliferation of blood vessels. The authors compared the therapeutic effects of islet cells transplanted from different sites in diabetic mice, including near the liver, subcutaneous, intestinal dermis, and abdominal adipose tissue.
For the currently commonly used liver transplantation, at least three donors of islet cells can meet the therapeutic effect of a patient. If researchers can reduce the amount of cells used, it will greatly promote the efficiency of islet transplantation and improve the Treatment effects in patients with diabetes. (Qijianbio, qijianbio)
Scan the QR code to read on your phone
Related News
Contact Us
Contact us


Contact Us
ADD: No.707 Chaofan street, High-Tech Industrial Development Zone, Changchun City, Jilin province, China
Service Hotline:0086-431-86561075
Fax:0086-431-88794098
Email:export@qijianbio.com
Copyright:Jilin Qijian Bio-pharmaceutical Co., Ltd. by:300.cn 吉ICP备20003293号 SEO